Face the Challenge of Provider Credentialing with Real-Time Updates
LexisNexis Provider Data Intelligence Suite tackles provider credentialing challenges for health plans.
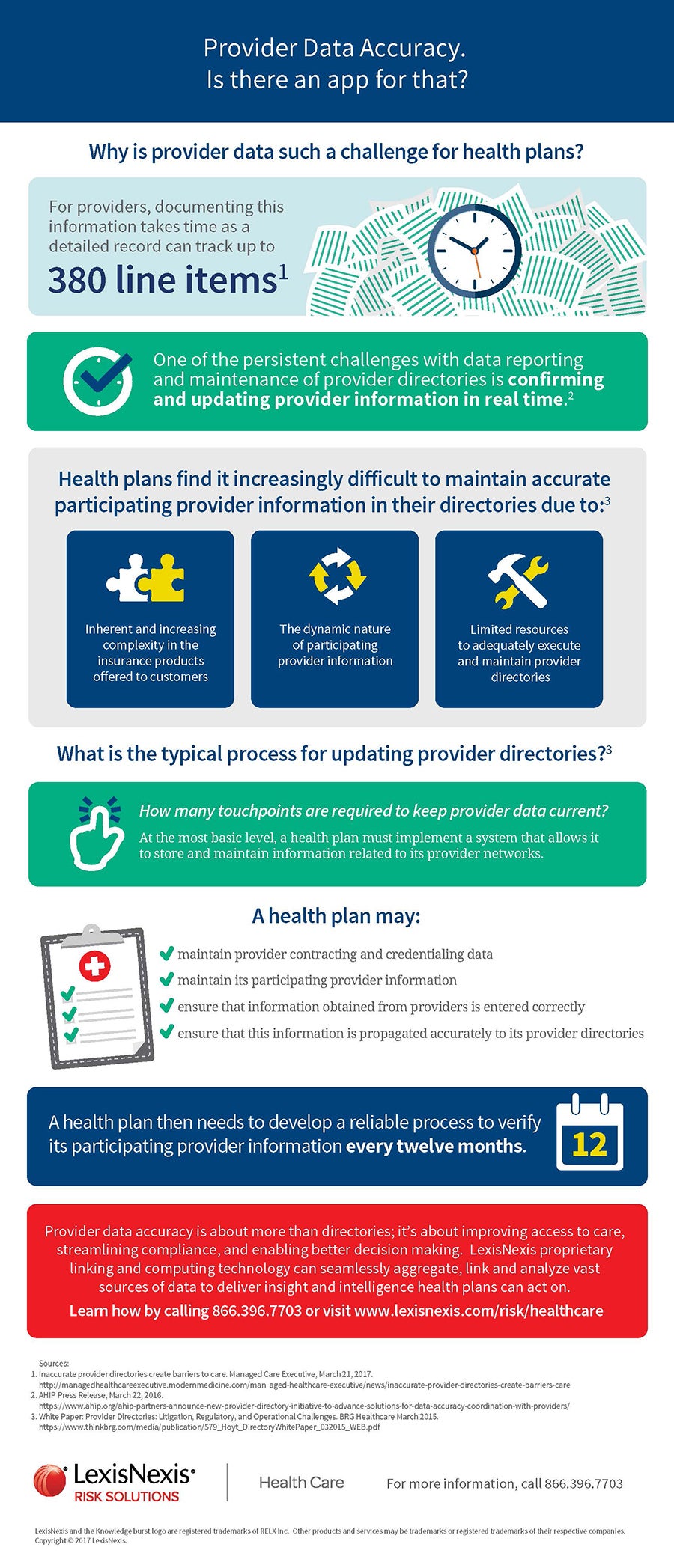
Provider credentialing and data accuracy goes beyond health plan directories; it's about improving access to care, compliance and decision making.
Health plans need to develop a reliable process to verify its participating provider credentialing and other data every twelve months. LexisNexis proprietary linking and computing technology can seamlessly aggregate, link and analyze vast sources of data to deliver insight and intelligence that health plans can use for their provider credentialing and other provider demographic verifications.
Access Full Infographic