Provider Data Validation
Real-time access to accurate, complete, and comprehensive provider information
LexisNexis Provider Data Validation is part of our Provider Data Intelligence Suite and the third stop along our provider data continuum.
Provider Data Validation is a web-based, real-time provider information search service that leverages the most current, comprehensive and accurate provider data.
It provides healthcare organizations with an efficient means to research new providers, health systems and affiliations to help claim/service operations, or assist with credentialing and provider data maintenance. Reliable and comprehensive provider data is essential to process claims and maintain workflows like network management, compliance, out-of-network provider screening and review, credentialing, and outreach. It helps healthcare organizations keep systems of record up to date and to fill in gaps in the existing data.
Provider data is constantly changing. Our data scientists have shown that:
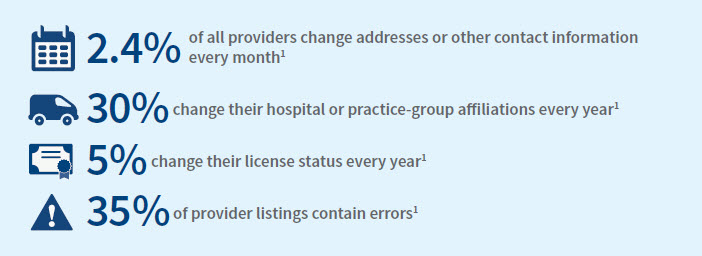
The process to maintain this information is complex and costly, from reconciling duplicate records to filling in missing data such as NPI numbers, contact information, sanctions and more. In each provider search, users can find detailed demographic data for healthcare providers.
Benefits
The LexisNexis Risk Solutions provider data repository is the most robust and up-to-date in the industry. By aggregating, cleansing and managing provider information, health plans, provider organizations, pharmacies and life sciences companies can make better decisions to help them meet their business goals and improve patient outcomes.
Features
Key features of LexisNexis Provider Data Validation include:
- Provider data expertise: LexisNexis is 1 of 2 companies in the U.S. that aggregate provider data from every state across U.S.
- Detailed, accurate and up-to-date demographic data for every provider, including:
- Provider status (e.g., deceased or retired)
- Company names and locations (including address, phone, fax and verification dates for that location)
- Group and hospital affiliations
- License number, state, type, status and end date
- DEA number, Business Activity Indicator and expiration or deactivation date
- Medical school and graduation year
- CMS specialty code
- Taxonomies (including Primary Indicator)
- Sanctions
- NPPES Health Care Provider Data (including NPI number and deactivation date)
Get it now: For more information about LexisNexis® Provider Data Validation, call 866.396.7703.
