
Are You Ready for the Public Health Emergency Unwinding?
Real World Data Puts the Pieces Together to Streamline Unwinding and Redetermination Decisions
Unprecedented Challenges Require Medicaid Organizations to Look Outside Their Data
During COVID, key demographic information required to identify, contact, and care for these individuals changed dramatically, leaving Medicaid agency’s records out-of-date.
With a nearly 20% increase in Medicaid applications/enrollment and complex policy landscapes, States must carefully balance the need to address their administrative redetermination backlogs – while still maintaining continuous coverage, administrative assistance and effective customer service for vulnerable populations.

Challenges of Unwinding
Unwinding redeterminations and revalidations for Medicaid benefits must coincide with regular processing of new Medicaid applications and increased Medicaid program rolls – generating volume spikes and pressures on limited existing staff.
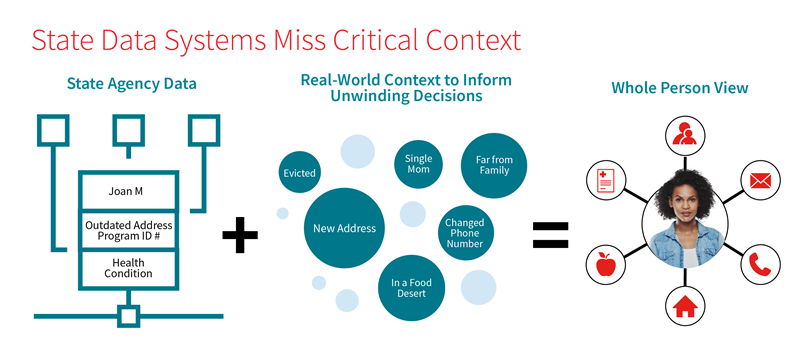
It’s not only about state agencies handling the increased volume of work. Inaccurate data can cause critical issues. Something as fundamental and incorrect or out of date as mailing addresses could put vulnerable seniors, pregnant women, and children at risk of losing coverage – and create administrative challenges for years to come. Incorrect data required for eligibility determination could result in wasted benefit dollars.
As the Public Health Emergency (PHE) extends, agency and department data sources will grow increasingly outdated — more people are getting back to work and receiving income, moving to new addresses, and experiencing other life changes that impact their data and whether or not they remain eligible for Medicaid benefits.
How serious is the problem?
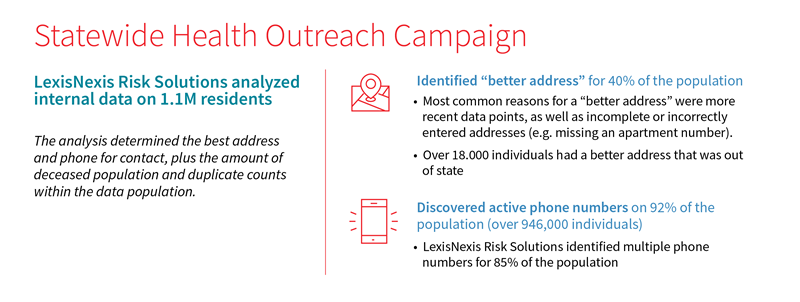
Even with the best outreach efforts, Medicaid organizations may fall short on preparedness when it comes to having the most up-to-date contact data to connect their eligible population to appropriate resources.
Over 11% of Americans have moved since the beginning of the pandemic. Underserved populations – such as the elderly, the poor and people with disabilities – are most likely to be impacted by relocation, as 20% of those who move said it was due to financial reasons or challenges affording housing.
Prior to starting unwinding processes, begin with a clean list.
Match data using a referential-based Master Person Index to link state data with thousands of real-world data sources – so that your organization can get the benefit of any name changes and accommodate for missing info or human typos.
To inform PHE Unwinding and redetermination decisions, agencies need real-world data from alternative sources to better understand each individual and enrollee. Alternative data sources are the key for agencies to truly understand the people they serve. Sensitive Medicaid program redetermination decisions require precise and timely insights.
• Continuously updated real-world data to understand member needs and context to improve coordination
of care.
• Fine-tune sensitive decisions with additional data and confidence scores.
• Applying the right data at the right time in the Medicaid Member lifecycle (and integrated into eligibility
LexisNexis® Risk Solutions brings more than 10,000+ sources of individual level public records and credit-based data to provide deeper insight and precision into understanding each individual and enrollee.
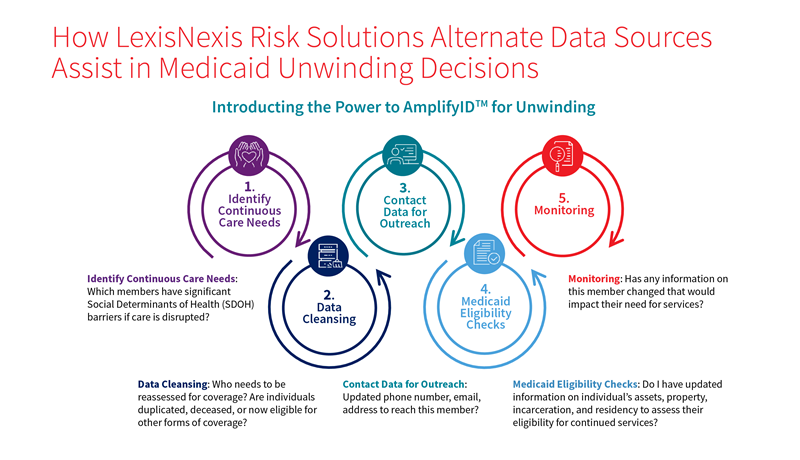
Streamline Eligibility Processes with Continuous Monitoring
Leveraging LexisNexis Risk Solutions data provides each state agency with the tools to help mitigate the risk of inappropriate terminations and churn, as well as ensure that the state also resumes timely processing of new applications. Enriching data by consolidating identities, removing, and flagging deceased or incarcerated individuals and enhancing the understanding of the populations served, are critical components of continuous care needs.
LexisNexis Risk Solutions can help overcome critical gaps by leveraging thousands of data sources to improve contact data, ensure consistency between departments, as well as determine what is most likely to be information critical for targeted outreach.
Understand & Prioritize Continuous Coverage through Real-World SDOH Data
Instead of relying on point-in-time social determinants of health (SDOH) assessments or zip code census data, Medicaid organizations can immediately unlock clinically validated data on each individual’s socioeconomic factors, such as housing instability, social isolation, food insecurity, or financial instability. LexisNexis® Socioeconomic Attributes and Scores provide agencies a population-level assessment of members’ SDOH profiles and relative risk for medication adherence gaps or readmission risks. Most importantly, LexisNexis Socioeconomic Scores provide agencies individual-level, ranked, SDOH care-drivers that point a care coordinator to specific SDOH care gaps that can be addressed to mitigate risk, speed renewals, and improve access.
Leveraging LexisNexis® AmplifyID™ for Unwinding greatly simplifies revalidations. Efficiency and ease of use are critical for Medicaid state agencies, particularly as Unwinding overlaps with regular processing of new Medicaid applications and increased program rolls.
AmplifyID™ for Unwinding accelerates understanding of the person at the core of unwinding decisions.
The AmplifyID for Unwinding Advantage: Tech + Data + People
Our HHS-focused solution architects and data analysts fine tune results to your specific workflow, system integration requirements, and policy preferences.
We work with you up-front and ongoing to determine:

How best to interpret and act on various types of contact data updates.

Policy goals and operational procedures to limit false positives and guide data-driven implementation.

How to prioritize or triage results according to your staff capabilities.

Technical integration capabilities and delivery mechanisms to dovetail with your systems.
Insights and Resources
Product Index
-
LexID® for Healthcare
Protect the identities of healthcare consumers.
-
Business Data Enrichment Suite
Optimize customer data to identify opportunities and avoid risk
-
Emailage® for Government
Add email intelligence as a layer of defense to fraud prevention.
-
AmplifyID™ Master Person Index
Ensure equitable access and smooth service delivery with a precise, whole-person view
-
Social Determinants of Health
Social Determinants of Health (SDOH) fuel insights into health risks and the ability to proactively impact health outcomes for veterans, military and others.
-
Account Monitoring
Receive automated alerts on key client information
-
Email Search
Confidently connect to consumers with industry-leading email intelligence.
-
Public Housing Integrity Scan
Analyze your resident population to reveal fraud, waste and abuse
-
Keep Contact
Transform your engagement efforts by improving and maintaining patient and member data.
-
Instant Verify
Verify IDs and professional credentials instantly
-
Multi-Factor Authentication for Healthcare
Authenticate members and providers
-
Provider Integrity Scan
Know your providers, reduce risk, and prevent fraud.
-
InstantID® Q&A
Authenticate customer identities in real-time








